Where can I get more information about best doctor for colonrectal treatment in Gurgram India?
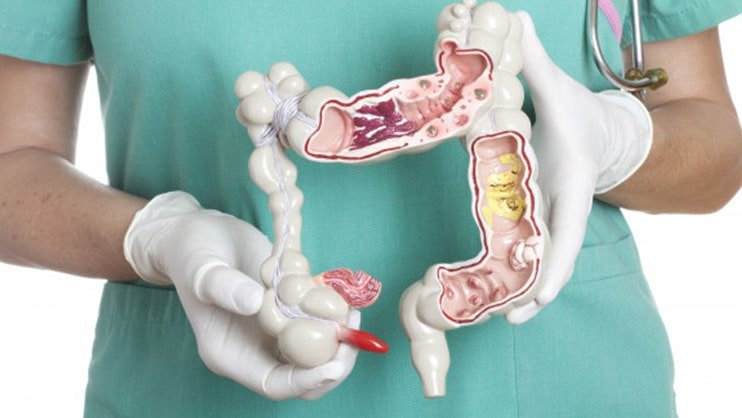
Colon and rectum are part of large intestine which is last portion of Gastrointestinal Tract/ digestive system. Cancer are called colon and rectal cancer depending upon part from which they are arising. They are groped together because they share may common features.
Large intestine is approx 1.5 meter long and most of part is colon. 1st part is ascending colon, small intestine continues in Caecum which is initial part of ascending colon. 2nd part is transverse colon, 3rd part is descending colon because it continues downward in 4th part called sigmoid colon. Sigmoid colon continues in last part of large intestine called rectum, most of which is deep in pelvis. Food nutrients get absorbed in small intestine and residue reaches in colon where water is absorbed. The stool formed is hold in rectum untill passed out through anus. Understanding of anal sphincter is very important in management of rectum cancer.
Colortectal cancers are 3rd most common and 2nd most common cause of cancer related mortality globally. In India it is 7th most common cancer group and 8th most common cause of cancer related mortality.
Risk factors
Age: More common beyond 45-50 years
Obesity/ overweight
Red meat/ processed meat consumption
Tobacco
Alcohol
Inflammatory bowel disease- anyone with inflammatory bowel disease need to start getting screened for colorectal cancer at early age and more often.
Family history of coloretacl cancer or polyp.
Personal history of colorectal cancer or Polyp
Abdominopelvic radiation exposure
Genetic Cancer Syndromes: Lynch syndrome (hereditary non-polyposis colorectal cancer, or HNPCC) and familial adenomatous polyposis (FAP)
Diet rich in fruits, vegetables, and whole grains, fibers and that limits or avoids red and processed meats and sugary drinks probably lowers risk.
Screening for Colorectal Cancer:
The American Cancer Society recommends that people with average risk should start regular screening at age 45. This can be done either with a stool based test to detect blood or by colonoscopy. People in good health should continue regular colorectal cancer screening up to 75 years. Between 76 - 85 years screening should be based on person’s preferences, overall health, and prior screening history. Beyond 85 years colorectal cancer screening usually not recommended.
Usually recommended tests are:
Highly sensitive guaiac-based fecal occult blood test (gFOBT) every year
Colonoscopy every 10 years
CT colonography (virtual colonoscopy) every 5 years
Flexible sigmoidoscopy (FSIG) every 5 years
For persons with high risk Screening is recommended to start early and more frequently with advise from treating doctor.
Alarming Signs
constipation
diarrhoea
changes in stool color
changes in stool shape, such as narrowed stool
blood in the stool
bleeding from the rectum
excessive gas
abdominal cramps
Unexplained weight loss, fatigue, loss of appetite
Difficulty in passing stool and gases. May cause intestinal obstruction if bulky growth.
Investigations
Colonoscopy and Biopsy
CECT/ MRI for disease extent evaluation
PET CECT may be advised in certain situation but not routinely required. CECT and MRI usually provided adequate information
Tumor markers: most commonly S. CEA (carcino embryonic antigen) is used. It also helps in followup.
Genetic testing may be advised in view of history details
Colonrectal Treatment In Gurgaon
Surgey: surgery is mainstay of treatment for colon and rectal cancer
Surgery for colon Cancer:
Radical Hemicolectomy with Intestinal anastomosis; is most commonly performed surgery which removes that segment of affected colon along with all lymph nodes and vascular supply and rejoin proximal and distal ends of intestine
Total coloectomy/ proctocolectomy: If multiple sites or associated multiple polyps and hereditary predisposing conditions.
Both Open and Minimal invasive approaches are used by surgical oncologist.
Surgery for Rectal cancer:
Low Anterior Resection: The cancer bearing Segment of rectum with adequate margin of normal tissue around the cancer is removed, along with nearby lymph nodes and other tissues around the rectum.The colon is then reattached to the remaining rectum
Short-term temporary stoma may be made in case of frail patients or difficult anastomosis. - end of the intestine is brought out through a hole in the skin of the abdomen. This gives the rectum time to heal before stool moves through it. Mostly stoma is reversed (the intestines reconnected) after adequate healing.
Intersphicteric resection: In case of very low lying cancer where external anal sphincter is safe from disease and has adequate tone and normal margin can be taken distally. Proximal colon is anastomosed to anal canal. Temporary stoma is required and revered after healing of anastomosis
Abdominoperineal Resection with Permanant Stoma: Cancer of lower part of the rectum or extending into anal canal, growing into the sphincter muscle (the muscle that keeps the anus closed and prevents stool leakage) or pelvic floor (called levator muscles). Also required in distal rectal cancer when sphicter muscle tone is poor.
Properly managed stoma give better quality of life than uncontrolled and poorly managed anal passage.
Metastatectomy: if colon or rectal cancer has spread to limited organ like Liver or lung and complete excision of metastasis is possible.
Cytoreductive surgery + Hyperthermic Intraperitoneal chemotherapy (CRS+HIPEC): when there is peritoneal (inner covering of abdomen) only metastasis extensive surgery is done to completely remove the disease followed by intraperitoneal instillation of heated chemotherapy during surgery.
Chemotherapy:
Usually given after surgery in advance colon cancer or cancer with high risk features for better long term control.
In large rectal cancer chemotherapy may be given before surgery (Neoadjuvant) mostly with Radiation or may be alone in certain cases. After surgery adjuvant chemotherapy is given for helping in better long term control.
In advance metastatic disease palliative chemotherapy is helpful.
Radiation therapy::
In large Rectal cancer Radiation therapy is given before surgery (neoadjuvant) for better long term control.
Targetted Therapy: have important role in advance metastatic disease.
Staging
Stage I: cancer is limited to various layers of colon or rectum wall.
Stage II: The cancer has grown through the wall of the colon or rectum to the lining of the abdomen, called the visceral peritoneum or directly invade nearby structures.
Stage III: The cancer has spread to lymph nodes
Stage IV: The cancer has spread to a distant part of the body, such as the liver or lungs.
Prognosis
| Stage | 5 years Survival |
|---|---|
| Localized (I+II) | 90% |
| Regional (III) | approx 70% |
| Stage IV | <15% |
| Overall | around 60% |
What Our Patients Say
Frequently Asked Questions
Colon cancer can start anywhere in the colon, which is about 5 feet long and absorbs water from the stool. Rectal cancer begins in the rectum, which is the last 12 cm (about 5 inches) of the colon. This is where the body defecates until you have a bowel movement. Contact Cancer Surgery Gurugram surgery gurugram for colon and rectal cancer treatment in Gurgaon.
"It is 10 times more likely to cause stomach cancer than rectal cancer, where it returns after treatment has begun." Colon cancer has about a 20 percent risk of local recurrence, versus about 2 percent with colon cancer. Contact Cancer Surgery Gurugram surgery gurugram for colon and rectal cancer treatment in Gurgaon.
Best Doctor for Rectal Cancer in Gurgaon says for rectal cancer, the overall 5-year survival rate for people is 67%. If the cancer is diagnosed locally, the survival rate is 89%. If the cancer has spread to surrounding tissues or organs and / or regional lymph nodes, the 5-year survival rate is 72%.
According to Best Doctor for Rectal Cancer in Gurgaon colorectal cancer is the third most common cancer found in the United States in both men and women, except for skin cancer. The American Cancer Society estimates for the number of colorectal cancer cases in the United States for 2021 are: 104,270 new cases of colon cancer. 45,230 new cases of rectal cancer.

